Design for life
With over 100 staff, we’re a passionate team of urban designers, landscape architects, architects, interior designers, digital experts, and sustainability advocates. We deliver design thinking to clients in industries from housing and retail to residential development, education, and aged care. By drawing together our multidisciplinary expertise and approaching problems from diverse perspectives, we answer our clients’ needs with originality, innovation, and relevance.
We have studios located in Newmarket and Kingsland (Auckland) along with Tauranga and Christchurch, giving us enough reach to service both the North and South Islands.
Our goal is simple, to help people live better lives – at home, in the workplace and when they’re out and about. With a focus on sustainability, we create future-proofed buildings and communities in context with their environments.
We exist to design for life.
Our work
Our team of designers work across all sectors, from aged care, residential developments, and affordable housing, through to retail, hospitality, and commercial. Visit our portfolio to see examples of our work.


Our commitment to sustainability
We believe in providing clients with informed choices about the best way to create buildings and places that perform. We aim to shift from creating buildings and environments that do less harm to places, to vibrant buildings and environments that serve to regenerate our world; socially, economically, and ecologically. Find out more about our sustainability commitment.


We integrate masterplanning, landscape, and architectural solutions to create successful, sustainable places that provide long-term value.

Our landscape architects' designs create ties to the land and a strong sense of place.

Our architectural service helps to transform our clients’ vision into successful, people-centric places. More

We provide innovative and creative interiors that enable a space to reach its full potential.
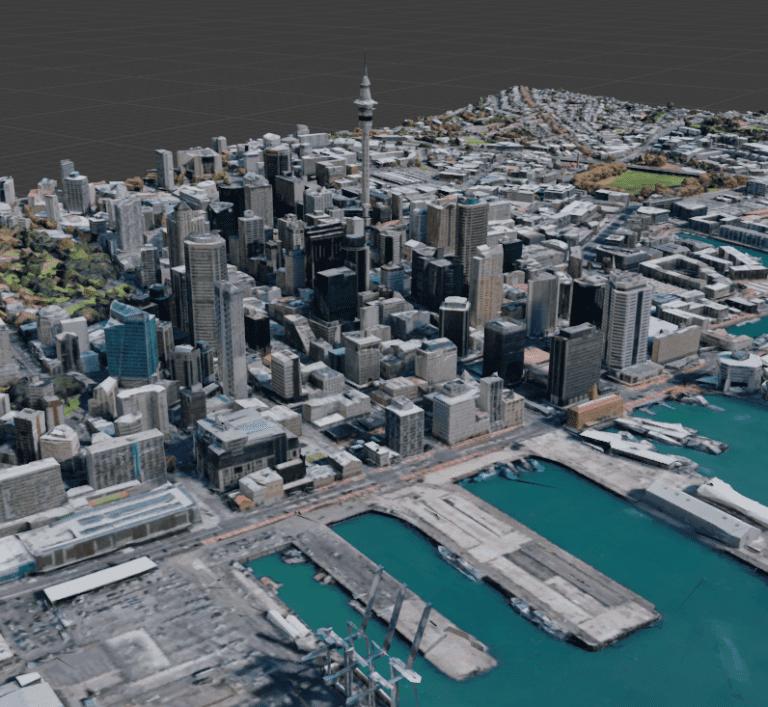
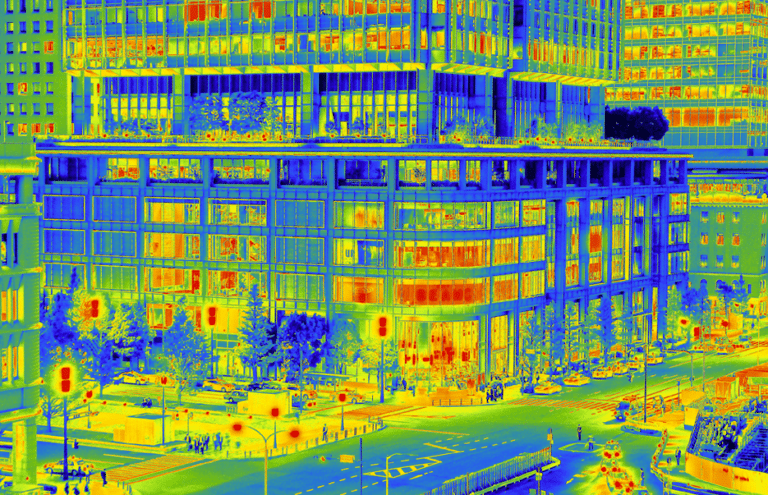
We offer VR, AR, 3D capture, BIMx, 3D printing and drone technology.

Our sustainability initiatives are incorporated across all of our services.
Context portal
Communication is the key to any successful project, which is why we created the Context portal. This online platform gives our clients access to their project’s status at any time, on any device. It provides the latest information on programmes, risks, issues, design documents, invoices, and statements – all in real-time.
Introducing our packaged services
We have created a suite of packages which are ideal for standard services and for those who need a fast and efficient turnaround. Click on the service to find out more.


Insights
Our affiliations




Got an idea for your next design project and need some help? Speak to one of our team of experts who’ll be happy to offer advice and support.